The blame narrative is fading
Those calling obesity a “personal choice” fell from 57% to 44%. More people now reject the idea of willpower as the cause, though men still lean toward blame more than women.
Obesity is still one of the UK’s most debated health issues, but public understanding hasn’t caught up with the science. Many still see weight as a personal failing, despite clear evidence that obesity is a complex medical condition. Our 2025 State of Obesity report tracks what’s shifted since last year, and what hasn’t.

The conversation around obesity has intensified in 2025, cutting across politics, pop culture, and healthcare. But the UK still faces one of the highest obesity rates in Europe and the economic cost now exceeds £126 billion. Despite this, 2025 marks the first time in two decades that national rates have begun to level off.
At the same time, public understanding is slowly catching up with the science: obesity isn't a matter of willpower but a complex, chronic disease shaped by biology. Building on last year’s report, we surveyed over 2,000 people, spoke to patients and clinicians, and reviewed emerging research to understand how attitudes are changing, and why accurate, accessible, science-based guidance is now more important than ever.
The data reveals five major cultural and behavioural shifts since 2024. These changes may be gradual, but together they show a clear movement away from outdated assumptions and toward a more scientific, compassionate understanding of obesity.
The blame narrative is fading
Those calling obesity a “personal choice” fell from 57% to 44%. More people now reject the idea of willpower as the cause, though men still lean toward blame more than women.
Medical framing is gaining ground
Fewer people deny obesity is a disease (29% vs. 43% last year), and strong opposition has collapsed from 18% to 7%. The view of obesity as a medical condition, and not a moral failing, is growing.
Medication has gone mainstream
Familiarity with GLP-1s has jumped from 37% to 49%, and nearly a quarter of adults have used them. Belief in their effectiveness tripled to 53%, while stigma is reversing: 41% now reject the idea that medication is “cheating.”
Biology is in conversation
High-calorie intake is now seen as the top driver of obesity (38%, up from 26%). Lifestyle explanations are falling, while recognition of biology and genetics has risen from 10% to 15%. The shift toward a medical model is growing, but still incomplete.
Stigma remains a major barrier
Despite progress, stigma is still the biggest obstacle to seeking help. 4 in 10 fear judgement, and over half of those living with obesity wish they could drastically change their weight, often feeling anxious, self-critical, or undeserving because of it.
Public attitudes toward obesity are beginning to shift, even if the change is subtle. Fewer people now see obesity as a simple matter of willpower, with belief in “personal choice” dropping sharply and more people recognising factors like biology and genetics.
The number of people who deny obesity is a disease has also fallen, while acceptance of the disease model is growing, especially among those living with obesity. Still, a large portion of the public remains unsure, reflecting a move away from blame but not yet toward full scientific understanding. Overall, the narrative is slowly evolving from discipline and dieting toward a clearer recognition of obesity as a complex, chronic condition shaped by biology, behaviour, and environment.
The belief that obesity is simply a “choice” is starting to lose ground, but it hasn’t disappeared. This year, 2 in 5 people still hold onto that view, even as the numbers fell sharply from 2024. What sits beneath this belief reveals a deeper divide in how the UK understands obesity: one side clinging to willpower and lifestyle, the other moving toward biology, complexity, and science.
| Measure | Agree that "obesity is a choice" | Disagree that "obesity is a choice" |
|---|---|---|
| % of the population | 44% (down from 57% in 2024) | 28% |
| Recognise obesity is a disease | 43% | 51% |
| Recognise genetics as a factor | 12% | 23% |
| See lack of exercise as a key cause | 44% | 29% |
| Believe regular walking is effective | 22% | 29% |
| Believe mindful eating is effective | 17% | 24% |
| Believe strength training is effective | 17% | 13% |
| Believe flexibility classes are effective | 15% | 10% |
Public attitudes are changing, even if it's not obvious at first glance.
67% said obesity was caused by personal behaviour
35% blamed fast food and sugary drinks
32% blamed sedentary lifestyles
38% still say overeating is the top cause
Only 17% point to lifestyle
Genetics recognition doubled from 7% to 15%
Fewer people now single out exercise or willpower
More people acknowledge biological and environmental factors
The “personal responsibility” narrative is weakening
A growing share of the UK now sees obesity as complex, and not simply a choice
Obesity is a recognised medical condition that affects the body far beyond the number on the scale. The World Health Organisation defines health as complete physical, mental, and social wellbeing, and obesity meets every part of that definition. It’s a chronic, complex disease that can disrupt hormones, increase the risk of serious conditions like type 2 diabetes, heart disease, and certain cancers, and impact everything from mobility to mental health.
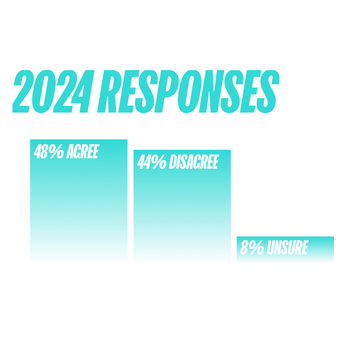
In 2024, views were almost evenly split. Nearly half of people (48%) agreed that obesity is a disease, while 44% disagreed. A small minority (just 8%) were unsure. This year’s baseline pie chart shows a nation caught between two narratives; one rooted in biology, the other still tied to personal responsibility and willpower. Strong opposition was also noticeably higher, with 18% firmly rejecting the disease model.

In 2025, agreement that obesity is a disease holds steady at 48%, but disagreement dropped sharply from 44% to 29%, and strong opposition has more than halved to just 7%. The biggest movement is in uncertainty: 27% now say they’re unsure, up from 8%, showing that while resistance is fading, many still need clearer guidance. Among those living with obesity, recognition is stronger, with 52% viewing it as a medical condition.
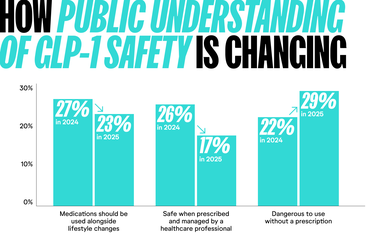
Public confidence in GLP-1 weight-loss medications is rising, and attitudes are becoming far more medically grounded. More people now say these treatments should be used alongside healthy lifestyle changes (27%) and that they’re safe when prescribed by a professional (25%), while 78% disagree that using them without a prescription is safe.
Compared with 2024, the conversation has shifted from fear to practicality, but beliefs still depend heavily on where people get their information. Those learning from trusted clinical sources show strong safety awareness, while those relying on unregulated online channels are more likely to hold risky views. As GLP-1s become mainstream, ensuring people receive accurate, evidence-based guidance is essential to keep treatment both effective and safe.

Public opinion is shifting, and it’s clear that people want more than personal-responsibility messaging. The public wants a system that supports real change, from affordable healthy food to accessible treatment, and not another round of blame or bureaucracy.
48%
Say that the UK government still isn't doing enough to tackle obesity.
56%
Of people who are overweight or living with obesity feel that current government action is insufficient.
39%
Want cheaper, more accessible healthy food as their top priority.
27%
Want better access to physical activity opportunities in their communities.
26%
Want more NHS-funded obesity services, rising to 35% among those with obesity.
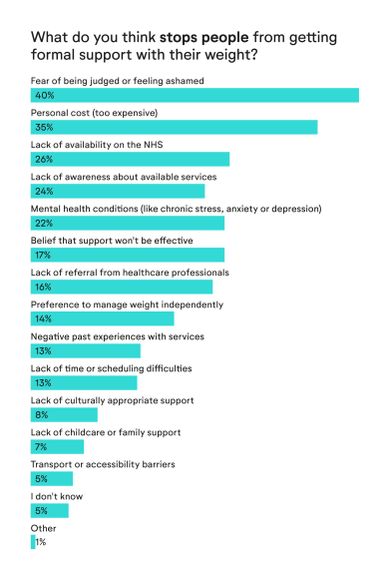
Weight stigma remains one of the biggest barriers to effective obesity care. Even as attitudes toward weight loss medication improve, many people still see obesity as a personal failing rather than a complex condition shaped by biology, environment, income, and mental health. When the narrative centres on willpower, shame takes over. People delay speaking to their GP, avoid asking about treatment, and convince themselves they should “just try harder.” Until we change how we talk about obesity, we’ll struggle to change how people feel about seeking help.
The accessibility gap deepens this problem. Fear of judgement is the number one reason people avoid support, followed closely by cost, limited NHS services, and a lack of awareness about what help actually exists. People aren’t asking for quick fixes; they’re asking for care that’s available, affordable, and free from shame. Creating that kind of environment is the foundation of effective obesity treatment.
Looking ahead to 2026, the conversation around obesity is set to shift from awareness to action. Public opinion is finally catching up with science, stigma is loosening its grip, and more people now view obesity as a medical condition rather than a personal failure. That momentum is likely to accelerate: recognition of obesity as a disease could reach a clear majority, GLP-1 treatments will continue their move into the mainstream through safe, regulated channels, and the moral backlash around medication will keep fading.
At the same time, pressure on policymakers will intensify. With many still believing the government isn’t doing enough, expect louder calls for affordable nutritious food, expanded NHS obesity services, and a more coordinated national approach. 2026 won’t just be another year of debate; it will be a test of whether the UK is ready to match public understanding with real change.
/)
This report is based on a nationally representative survey of 2,000 UK adults, commissioned by Numan and carried out by Attest in October 2025. Respondents were recruited and verified through Attest’s online panel, with quotas set to match UK demographics across age, sex, region, and body-weight categories. All responses were anonymous, and the final data was weighted to reflect the wider population. Results were analysed using standard statistical methods, with findings reported at an 85–95% confidence level and a margin of error of ±3.1%.
Updated: